Many patients with diabetes develop extremely dry, cracking skin which makes it much more susceptible to infection. In fact, approximately 70% of surgical amputations done in Canada are performed on diabetes patients who have developed infections through cracks or breaks in extremely dry skin.
Why is diabetes associated with poor skin health?
1. Diabetes is linked to thickening of the skin.
2. Diabetes leads to reduced blood circulation to the skin (microangiopathy).
3. Increased frequency of urination reduces the moisture available for the skin.
4. Researchers believe that the body may actually “rob” the skin of moisture to eliminate glucose from the tissue.
The first symptoms of compromised skin health are often dry, scaly skin that can appear anywhere on the body but is most common at the extremities including: legs, feet, knees, elbows and hands. This is a common condition among patients with diabetes and results in less supple skin that can crack easily.
Be aware of skin cracks and infection
Skin cracks open the door for bacteria, viruses and fungi to enter our bodies, often leading to open sores and infections.
Reduced or delayed healing
Not only is the skin more susceptible to infection, it is generally slower to heal. So patients with diabetes face the compounding problems of being more prone to infection and being much slower to heal once infection has occurred. Four factors contribute to the slower healing rate: reduced blood flow to the skin, higher blood glucose which supports bacterial growth, slower metabolic rate and thicker skin.
Thick Skin
Intact normal skin is the best barrier to infection. Thickened skin common to diabetics makes skin more susceptible to infection. A useful analogy might be to compare the water restraining ability of clay with pebbles.
How healthy is your skin?
Take this healthy skin test. There are six warning signs that your skin’s ability to resist infection has weakened.
- Has your skin grown noticeably thicker?
- Has your skin become more yellow in colour?
- Is your skin noticeably drier?
- Is your skin becoming scaly?
- Is your skin cracking?
- Do you notice that minor wounds take longer to heal?
If you answered yes to any of these questions you should make improved skin care an immediate priority.
Talk to your physician or diabetes nurse educator for more information about skin care and the best moisturizers to use.
Skin care guide
Healthy skin is supple, smooth and well hydrated, in other words, has plenty of moisture. It not only looks and feels better, but most importantly, healthy skin is your best defence against infection.
Here are 6 simple suggestions to help you maintain good skin health.
Practice good diabetes management
Fluctuations in blood glucose levels can stress your overall health, including your skin health.
Hydrate your body
Make sure you drink plenty of water.
Hydrate your skin
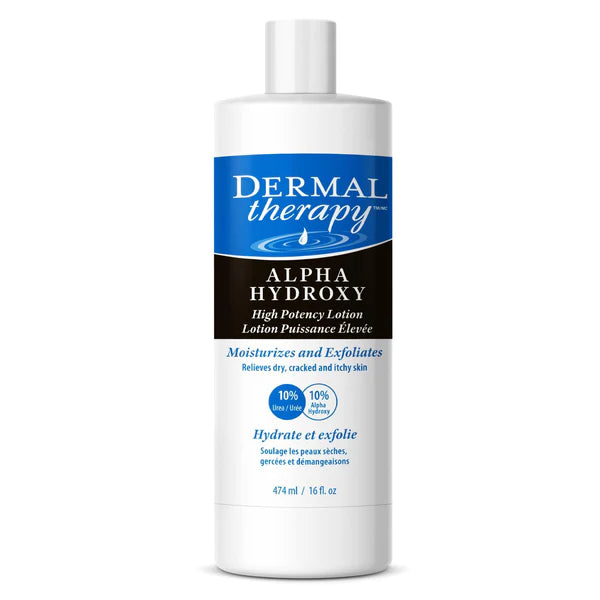
Use a moisture-replenishing lotion. Most creams and lotions just coat your skin to trap moisture. It is important to use moisture-replenishing products that contain ingredients such as UREA. The best time to apply these moisturizers is after bathing.
Dress Properly
Avoid excessive exposure to wind and sun by using hats, long sleeves and lotions to protect your skin. In winter your skin is particularly vulnerable to dryness so take extra care.
Be careful
Be extra careful to treat minor wounds such as blisters, cuts, abrasions and scratches with appropriate creams or ointments without delay.
Pay special attention to your feet
Your feet are particularly prone to problem skin and infections. Very good moisturizers are available that are formulated specifically for feet and heels. Never put moisturizers between your toes - it’s an area that already tends to trap heat and moisture, which creates a breeding ground for fungus and bacteria.
Diabetes links
Juvenile Diabetes Research Foundation International
Diabetes Public Health Resource - CDC
International Diabetes Federation